Approach Considerations
In the 1980s, many experts felt that urine cultures were unnecessary in young women with probable cystitis because almost all of these were caused by pan-susceptible isolates of Escherichia coli. Since then, however, antibiotic resistance in uropathogenic E coli has become a significant concern. Resistance also has been emerging among other common cystitis pathogens, including Enterococcus faecalis, Staphylococcus saprophyticus, Klebsiella pneumoniae, and Proteus mirabilis.
Trimethoprim-sulfamethoxazole (TMP-SMX) resistance reached levels as high as 20% prior to COVID-19. Substitution of fluoroquinolones had led to an increase in resistance to these drugs, as well. [16]
Nevertheless, according to 2010 guidelines from the American College of Obstetricians and Gynecologists, a urine culture is not required for the initial treatment of women with a symptomatic lower urinary tract infection (UTI) with pyuria or bacteriuria or both. [17] In a UK study, dipstick diagnosis proved more cost-effective than positive midstream urine culture for targeting antibiotic therapy. [5]
During the COVID -19 epidemic, there has been an outstanding increase in a variety of bacterial and fungal cultiures. [18, 19, 20]
Urine cultures should be obtained in all cases of cystitis in immunosuppressed patients and in those with a recent history of instrumentation, exposure to antibiotics, or recurrent infection. Obtaining cultures also is advisable in elderly women, who have a high rate of upper tract involvement.
Microscopic hematuria is found in about half of cystitis cases; when found without symptoms or pyuria, it should prompt a search for malignancy. Other possibilities to be considered in the differential diagnosis include calculi, vasculitis, renal tuberculosis, and glomerulonephritis.
In a developing country, hematuria is suggestive of schistosomiasis. Retention of Schistosoma haematobium eggs and formation of granulomas in the urinary tract can lead not only to hematuria but also to dysuria, bladder polyps and ulcers, and even obstructive uropathies. Schistosomiasis also can be associated with salmonellosis and squamous cell malignancies of the bladder.
Bacteremia is associated with pyelonephritis, corticomedullary abscesses, and perinephric abscesses. Approximately 10-40% of patients with pyelonephritis or perinephric abscesses have positive results on blood culture. Bacteremia is not necessarily associated with a higher morbidity or mortality in women with uncomplicated UTI.
Cervical swabs may be indicated in cases of possible pelvic inflammatory disease.
Visual inspection of the urine is not helpful. Cloudiness of the urine most often is due to protein or crystal presence, and malodorous urine may be due to diet or medication use.
No imaging studies are indicated in the routine evaluation of cystitis. Renal function testing is not indicated in most episodes of UTI, but it may be helpful in patients with known urinary tract structural abnormality or renal insufficiency. Renal function testing also may be helpful in older, particularly ill-appearing hosts or in hosts with other complications.
A study of 196 women with painful and/or frequent urination found that most could be classified as having a low or high risk for UTI by asking the following questions [21, 22] :
-
Does the patient think they have a UTI?
-
Is there at least considerable pain on urination?
-
Is there vaginal irritation?
History correctly classified 56% of patients as having a UTI risk of either less than 30% or more than 70%, and adding urine dipstick results increased this correct classification rate to 73%. Correct classification increased to 83% when patients with intermediate risk (30-70%) after history alone underwent an additional test. The strongest indicators of UTI were the patient's suspicion of having a UTI and a positive nitrite test. [21, 22]
Urinalysis
The most accurate method to measure pyuria is counting leukocytes in unspun fresh urine using a hemocytometer chamber; greater than 10 white blood cells (WBCs)/mL is considered abnormal. Counts determined from a wet mount of centrifuged urine are not reliable measures of pyuria. A noncontaminated specimen is suggested by a lack of squamous epithelial cells. Pyuria is a sensitive (80-95%) but nonspecific (50-76%) sign of UTI.
White cell casts may be observed in conditions other than infection and may not be present in all cases of pyelonephritis. A spun sample (5 mL at 2000 revolutions per min [rpm] for 5 min) is best used for evaluation of cellular casts.
Proteinuria commonly is observed in infections of the urinary tract, but the proteinuria usually is low grade. More than 2 g of protein per 24 hours suggests glomerular disease.
Approximately 70% of patients with corticomedullary abscesses have abnormal urinalysis findings, whereas those with renal cortical abscesses usually have normal findings. Two thirds of patients with perinephric abscesses have an abnormal urinalysis.
Urine specimen collection
Urine specimens may be obtained by midstream clean catch, suprapubic aspiration, or catheterization.
The midstream-voided technique is as accurate as catheterization if proper technique is followed. Instruct the woman to remove her underwear and sit facing the back of the toilet. This promotes proper positioning of the thighs.
Instruct the patient to spread the labia with one hand and cleanse from front to back with povidone-iodine or soaped swabs with the other hand; then pass a small amount of urine into the toilet; and finally urinate into the specimen cup. The use of a tampon may allow a proper specimen if heavy vaginal bleeding or discharge is present.
Midstream urine specimens may become contaminated, particularly if the woman has difficulty spreading and maintaining separation of the labia. The presence of squamous cells and lactobacilli on urinalysis suggests contamination or colonization (see image below). Catheterization may be needed in some women to obtain a clean specimen, although it poses the risk for iatrogenic infection. [23]
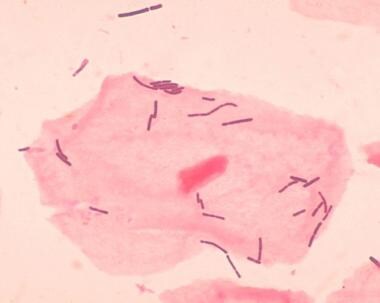 Lactobacilli and a squamous epithelial cell are evident on this vaginal smear. The presence of squamous cells and lactobacilli on urinalysis suggests contamination or colonization. Source: Centers for Disease Control and Prevention, Dr. Mike Miller
Lactobacilli and a squamous epithelial cell are evident on this vaginal smear. The presence of squamous cells and lactobacilli on urinalysis suggests contamination or colonization. Source: Centers for Disease Control and Prevention, Dr. Mike Miller
Although the use of midstream urine specimens is widely advocated, one randomized trial in young women showed that the rate of contamination was nearly identical among those who used midstream clean-catch technique and those who urinated into a container without cleansing the perineum or discarding the first urine output. Use of a vaginal tampon in addition to clean-catch technique had no significant effect on the contamination rate. [24]
Dipstick testing
Dipstick testing should include glucose, protein, blood, nitrite, and leukocyte esterase. Leukocyte esterase is a dipstick test that can rapidly screen for pyuria; it is 57-96% sensitive and 94-98% specific for identifying pyuria. Given this broad range of sensitivity, it is important to consider the possibility of false-positive results, particularly with asymptomatic patients undergoing evaluation for recurrent UTI.
Pyuria, as indicated by a positive result of the leukocyte esterase dipstick test, is found in the vast majority of patients with UTI. This is an exceedingly useful screening examination that can be performed promptly in any ED setting. If pyuria is absent, the diagnosis of UTI should be questioned until urine culture results become available.
In a United Kingdom study, dipstick diagnosis based on findings of nitrite or both leukocyte esterase and blood was 77% sensitive and 70% specific, with a positive predictive value of 81% and a negative predictive value of 65%. [5] Diagnosis on clinical grounds proved less sensitive.
Urine microscopy
A microscopic evaluation of the urine sample for WBC counts, RBC counts, and cellular or hyaline casts should be performed. In the office, a combination of clinical symptoms with dipstick and microscopic analysis showing pyuria and/or positive nitrite and leukocyte esterase tests can be used as presumptive evidence of UTI.
Low-level pyuria (6-20 WBCs per high-power field [hpf] microscopy on a centrifuged specimen) may be associated with an unacceptable level of false-negative results with the leukocyte esterase dipstick test, as Propp et al found in an ED setting. [25]
In females with appropriate symptoms and examination findings suggestive of UTI, urine microscopy may be indicated despite a negative result of the leukocyte esterase dipstick test. Current emphasis in the diagnosis of UTI rests with the detection of pyuria. As noted, a positive leukocyte esterase dipstick test suffices in most instances.
According to Stamm et al, levels of pyuria as low as 2-5 WBCs/hpf in a centrifuged specimen are important in females with appropriate symptoms. The presence of bacteriuria is significant. However, the presence of numerous squamous epithelial cells raises the possibility of contamination. [23] Low-level or, occasionally, frank hematuria may be noted in otherwise typical UTI; however, its positive predictive value is poor.
Nitrite test
Nitrite tests detect the products of nitrate reductase, an enzyme produced by many bacterial species. These products are not present normally unless a UTI exists. This test has a sensitivity and specificity of 22% and 94-100%, respectively. The low sensitivity has been attributed to enzyme-deficient bacteria causing infection or low-grade bacteriuria.
A positive result on the nitrite test is highly specific for UTI, typically because of urease-splitting organisms, such as Proteus species and, occasionally, E coli; however, it is very insensitive as a screening tool, as only 25% of patients with UTI have a positive nitrite test result.
Urine Culture
Urine culture remains the criterion standard for the diagnosis of UTI. Collected urine should be sent for culture immediately; if not, it should be refrigerated at 4°C. Two culture techniques (dip slide, agar) are widely used and accurate.
The 2010 Infectious Disease Society of America (IDSA) consensus limits for cystitis and pyelonephritis in women are more than 1000 colony-forming units (CFU)/mL and more than 10,000 CFU/mL, respectively, for clean-catch midstream urine specimens. Historically, the definition of UTI was based on the finding at culture of 100,000 CFU/mL of a single organism. However, this misses up to 50% of symptomatic infections, so the lower colony rate of greater than 1000 CFU/mL now is accepted. [26]
The definition of asymptomatic bacteriuria still uses the historical threshold. Asymptomatic bacteruria in a female is defined as a urine culture (clean-catch or catheterized specimen) growing greater than 100,000 CFU/mL in an asymptomatic individual.
Note that any amount of uropathogen grown in culture from a suprapubic aspirate should be considered evidence of a UTI. Approximately 40% of patients with perinephric abscesses have sterile urine cultures.
An uncomplicated UTI (cystitis) does not require a urine culture unless the woman has experienced a failure of empiric therapy. Obtain a urine culture in patients suspected of having an upper UTI or a complicated UTI, as well as those in whom initial treatment fails.
If the patient has had a UTI within the last month, relapse probably is caused by the same organism. Relapse represents treatment failure. Reinfection occurs in 1-6 months and usually is due to a different organism (or serotype of the same organism). Obtain a urine culture for patients who are reinfected.
If a Gram stain of an uncentrifuged, clean-catch, midstream urine specimen reveals the presence of 1 bacterium per oil-immersion field, it represents 10,000 bacteria/mL of urine. A specimen (5 mL) that has been centrifuged for 5 minutes at 2000 rpm and examined under high power after Gram staining will identify lower numbers. In general, a Gram stain has a sensitivity of 90% and a specificity of 88%.
Complete Blood Cell Count
A CBC is not helpful in differentiating upper from lower UTI or in making decisions regarding admission. Significant leukopenia in hosts who are older or immunocompromised may be an ominous finding.
The WBC count may or may not be elevated in patients with uncomplicated UTI, but it usually is elevated in patients with complicated UTIs. Patients with complicated UTIs may have anemia; for example, anemia is observed in 40% of patients with perinephric abscesses.
Diagnostic Catheterization
Catheterization is indicated if the patient cannot void spontaneously, if the patient is too debilitated or immobilized, or if obesity prevents the patient from obtaining a suitable specimen. Measurement of postvoiding residual urine volume by catheterization may reveal urinary retention in a host with a defective bladder-emptying mechanism.
Measurement of the postvoid residual volume should be strongly considered in all patients who require hospital-level care. Handheld portable bladder scans also may be used as a noninvasive alternative.
Guidelines from the Centers for Disease Control and Prevention (CDC) advise that in acute care hospital settings, aseptic technique and sterile equipment for catheter insertion must be used to minimize the risk for catheter-associated UTI. Only properly trained individuals who are skilled in the correct technique of aseptic catheter insertion and maintenance should take on this task. [27]
For more information on this procedure, see the Medscape Reference article Urethral Catheterization in Women.
Patients with Spinal Cord Injury
Diagnosing a UTI in a patient with a spinal cord injury is difficult. In these patients, signs and symptoms suggestive of a UTI are malodorous and cloudy urine, muscular spasticity, fatigue, fevers, chills, and autonomic instability.
In these patients, suprapubic aspiration of the bladder is the criterion standard for diagnosing a UTI, although it is not performed often in clinical practice.
For more information on this topic, see the Medscape Reference article Urinary Tract Infections in Patients with Spinal Cord Injury.
Patients with Diabetes Mellitus
Patients with diabetes are at risk for complicated UTIs, which may include renal and perirenal abscess, emphysematous pyelonephritis, emphysematous cystitis, fungal infections, xanthogranulomatous pyelonephritis, and papillary necrosis.
For more information, see the Medscape Reference topic Urinary Tract Infections in Diabetes Mellitus.
Cystitis Caused by Candida
Cystitis caused by Candida is clinically similar to cystitis from other pathogens. The presence of fungus in the urine should be verified by repeating the urinalysis and urine culture. Other features of diagnosis are as follows [28] :
-
Pyuria is a nonspecific finding
-
C glabrata may be differentiated from other species by morphology
-
Candida casts in the urine indicate renal candidiasis but rarely are seen
-
Colony counts have not proved diagnostically useful
Ultrasonography of the kidneys and collecting systems is the preferred initial study in symptomatic or critically ill patients with candiduria, but computed tomography is better for detecting pyelonephritis or perinephric abscess. [28]
-
Nonobstructing distal left ureteral calculus 2 X 1 X 2 cm.
-
Multiple abscesses, upper pole of left kidney.
-
Bilateral hydronephrosis.
-
Plain radiograph in a 63-year-old patient with poorly controlled type 2 diabetes mellitus shows emphysematous cystitis.
-
Lactobacilli and a squamous epithelial cell are evident on this vaginal smear. The presence of squamous cells and lactobacilli on urinalysis suggests contamination or colonization. Source: Centers for Disease Control and Prevention, Dr. Mike Miller
Tables
What would you like to print?
- Overview
- Presentation
- DDx
- Workup
- Treatment
- Approach Considerations
- Uncomplicated Cystitis in Nonpregnant Patients
- Complicated Cystitis in Nonpregnant Women
- Antimicrobial Therapy
- Adjunctive Therapy
- Fungal Infection
- Treatment in Patients with Spinal Cord Injury
- Pregnant Patients
- Renal Transplantation Patients
- Asymptomatic Bacteriuria
- Diet
- Consultations
- Prevention and Long-Term Monitoring
- Show All
- Guidelines
- Medication
- Media Gallery
- Tables
- References

